Pilonidal cysts represent one of the most challenging conditions affecting the sacrococcygeal region, causing significant discomfort and disruption to daily activities. These fluid-filled sacs, typically located in the natal cleft between the buttocks, affect over 70,000 individuals annually in the United States alone. The pain associated with pilonidal cysts can range from mild discomfort during sitting to excruciating agony that renders normal movement nearly impossible. Understanding the nature of this pain, its underlying mechanisms, and effective management strategies is crucial for both patients and healthcare providers navigating this complex condition.
Pilonidal cyst pathophysiology and pain mechanisms
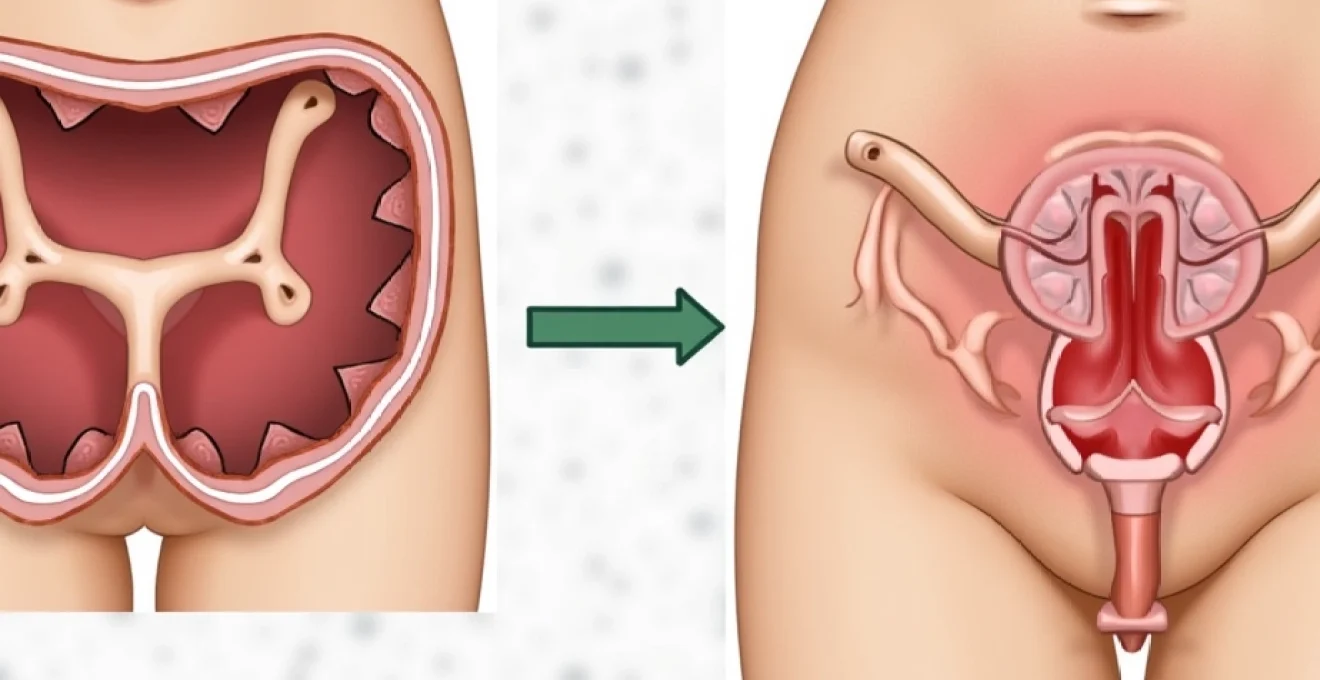
The development of pilonidal cysts involves a complex interplay of anatomical predisposition, mechanical factors, and inflammatory responses. The sacrococcygeal region’s unique anatomy creates an environment prone to hair penetration and subsequent cyst formation. When loose hairs become embedded in the skin through friction and pressure, the body initiates an immune response, forming a protective barrier around the foreign material.
Keratin debris accumulation in natal cleft hair follicles
The accumulation of keratin debris within natal cleft hair follicles serves as the initial trigger for pilonidal cyst development. Keratin , a structural protein found in hair and skin cells, combines with sebaceous secretions to create a viscous mixture that can obstruct follicular openings. This obstruction leads to follicular distension and eventual rupture, allowing hair shafts to penetrate deeper into the subcutaneous tissue. The presence of foreign keratin material triggers a localised inflammatory response, characterised by increased vascular permeability and immune cell recruitment.
Inflammatory cascade progression from acute to chronic stages
The inflammatory cascade in pilonidal disease progresses through distinct phases, each contributing to the overall pain experience. During the acute phase, pro-inflammatory mediators such as interleukin-1β and tumour necrosis factor-α are released, causing vasodilation and increased tissue sensitivity. This inflammatory soup directly stimulates nociceptors, leading to the characteristic throbbing pain associated with active pilonidal cysts. As the condition transitions to a chronic state, persistent inflammation results in tissue remodelling and the formation of fibrous scar tissue, which can contribute to ongoing discomfort even in the absence of active infection.
Neuropathic pain development through sacrococcygeal nerve involvement
The sacrococcygeal region is richly innervated by branches of the posterior cutaneous nerve of the thigh and the coccygeal nerve plexus. Chronic inflammation associated with pilonidal disease can lead to nerve sensitisation and neuropathic pain development. This type of pain is often described as burning, shooting, or electric-like sensations that may radiate beyond the immediate cyst area. Nerve compression from inflammatory swelling or scar tissue formation can result in allodynia, where normally non-painful stimuli become painful, making simple activities like sitting or wearing clothing uncomfortable.
Bacterial colonisation patterns: staphylococcus aureus and anaerobic species
Bacterial colonisation plays a crucial role in pilonidal cyst pain progression and intensity. Staphylococcus aureus represents the most common pathogen isolated from infected pilonidal cysts, with studies showing its presence in approximately 60% of cases. Anaerobic species, including Bacteroides fragilis and Peptostreptococcus, thrive in the low-oxygen environment of deep cysts and contribute to the characteristic foul-smelling discharge. These bacterial populations produce toxins and enzymes that directly damage tissue and amplify the inflammatory response, resulting in increased pain intensity and prolonged healing times.
Clinical pain assessment using validated measurement tools
Accurate pain assessment in pilonidal disease requires a comprehensive approach utilising validated measurement tools and clinical examination techniques. The subjective nature of pain makes standardised assessment crucial for treatment planning and monitoring therapeutic outcomes. Healthcare providers must consider both the intensity and quality of pain, as well as its impact on functional activities and quality of life.
Visual analogue scale (VAS) implementation for pilonidal cyst discomfort
The Visual Analogue Scale remains the gold standard for quantifying pilonidal cyst pain intensity in clinical practice. This 10-centimetre horizontal line, anchored by “no pain” and “worst possible pain,” allows patients to mark their current pain level with precision. Research indicates that pilonidal cyst patients typically report VAS scores between 4-8 during acute episodes, with sitting-related pain often scoring higher than resting discomfort. The VAS proves particularly valuable for monitoring treatment response, as successful interventions typically result in a 30-50% reduction in scores within the first week of appropriate management.
Mcgill pain questionnaire applications in sacrococcygeal region assessment
The McGill Pain Questionnaire provides a multidimensional approach to pilonidal cyst pain assessment, capturing both sensory and affective components of the pain experience. Patients with pilonidal disease commonly select descriptors such as “throbbing,” “burning,” and “tender” from the sensory category, while “tiring” and “annoying” frequently appear in the affective domain. This comprehensive assessment tool helps clinicians understand the pain’s impact on emotional well-being and daily functioning, informing both pharmacological and non-pharmacological treatment approaches.
Pilonidal disease activity index (PDAI) scoring system
The Pilonidal Disease Activity Index represents a specialised assessment tool designed specifically for evaluating disease severity and treatment outcomes in pilonidal conditions. This comprehensive scoring system incorporates pain intensity, discharge characteristics, inflammation signs, and functional limitations into a single numerical score. PDAI scores range from 0-45, with higher scores indicating more severe disease activity. Clinical studies demonstrate strong correlations between PDAI scores and patient-reported quality of life measures, making this tool valuable for both clinical assessment and research applications.
Differential diagnosis: distinguishing from perianal abscess and tailbone trauma
Accurate differential diagnosis is essential for appropriate pain management in pilonidal disease, as several conditions can mimic its presentation. Perianal abscesses typically occur closer to the anal verge and are associated with different bacterial flora and drainage patterns. Tailbone trauma, or coccydynia, presents with pain primarily during sitting and standing transitions, without the characteristic sinus tracts or hair-filled cysts of pilonidal disease. Hidradenitis suppurativa may also occur in the gluteal cleft but typically involves multiple interconnected sinuses and affects other body regions, helping to distinguish it from isolated pilonidal disease.
Conservative pain management strategies and interventions
Conservative management approaches form the cornerstone of initial pilonidal cyst pain treatment, particularly for uncomplicated cases without signs of severe infection. These strategies focus on reducing inflammation, promoting drainage, and preventing further hair penetration while addressing immediate pain relief needs. The effectiveness of conservative measures depends largely on early intervention and patient compliance with recommended protocols.
Warm sitz baths represent one of the most beneficial conservative interventions for pilonidal cyst pain management. Soaking the affected area in warm water for 15-20 minutes, three to four times daily, promotes vasodilation and natural drainage while providing immediate pain relief. The warmth helps reduce muscle tension in the gluteal region and can facilitate the spontaneous drainage of superficial abscesses. Adding Epsom salts to the bath water may provide additional anti-inflammatory benefits, though evidence for this practice remains largely anecdotal.
Proper positioning and activity modification play crucial roles in conservative pain management. Patients should avoid prolonged sitting on hard surfaces and consider using specialised cushions with coccygeal cutouts to reduce pressure on the affected area. Side-lying positions during rest and sleep can significantly reduce discomfort compared to sitting or lying on the back. When sitting is unavoidable, frequent position changes every 30 minutes help prevent sustained pressure that can exacerbate pain and inflammation.
Hair removal strategies, while primarily preventative, can also contribute to pain reduction in active cases. Regular hair removal from the natal cleft area using depilatory creams or professional laser treatment reduces the likelihood of additional hair penetration and subsequent cyst formation. However, shaving should be avoided during active inflammation, as it may introduce additional bacteria and cause micro-trauma to already compromised tissue.
Conservative management approaches can provide significant pain relief in up to 70% of patients with uncomplicated pilonidal disease, making them an essential first-line treatment option.
Pharmacological pain control protocols
Pharmacological interventions for pilonidal cyst pain management require a multimodal approach addressing both nociceptive and inflammatory components of the pain experience. The selection of appropriate medications depends on pain severity, infection status, patient comorbidities, and individual response patterns. Evidence-based protocols emphasise the importance of combining different drug classes to achieve optimal pain control while minimising adverse effects.
Nsaids selection: ibuprofen vs diclofenac efficacy profiles
Non-steroidal anti-inflammatory drugs form the foundation of pharmacological pain management in pilonidal disease, offering both analgesic and anti-inflammatory properties. Ibuprofen , administered at doses of 400-600mg every 6-8 hours, provides effective pain relief for mild to moderate pilonidal cyst discomfort. Its favourable side effect profile and over-the-counter availability make it an excellent first-line choice for most patients. Diclofenac, available in both oral and topical formulations, offers superior anti-inflammatory potency but carries a higher risk of gastrointestinal complications. Clinical studies suggest that diclofenac 50mg twice daily may provide better pain control than equivalent ibuprofen doses in patients with severe inflammation, though individual response varies significantly.
Topical analgesics: lidocaine and benzocaine application techniques
Topical anaesthetics provide localised pain relief without systemic side effects, making them valuable adjuncts to oral medications. Lidocaine 5% ointment, applied to the affected area 2-3 times daily, can provide 2-4 hours of significant pain reduction. The application technique involves gentle cleansing of the area followed by a thin layer of ointment, avoiding excessive pressure that might worsen discomfort. Benzocaine preparations , while effective for superficial pain, may cause contact sensitisation in some patients and should be used with caution. Combination preparations containing both lidocaine and anti-inflammatory agents show promise in clinical trials but are not yet widely available.
Antibiotic therapy: clindamycin and Trimethoprim-Sulfamethoxazole protocols
Antibiotic therapy becomes essential when pilonidal cysts develop secondary bacterial infections, contributing significantly to pain reduction through inflammation control. Clindamycin 300mg three times daily for 7-10 days provides excellent anaerobic coverage and good tissue penetration in the gluteal region. This antibiotic proves particularly effective against the mixed bacterial populations commonly found in infected pilonidal cysts. Trimethoprim-sulfamethoxazole, dosed at 160/800mg twice daily, offers broad-spectrum coverage including methicillin-resistant Staphylococcus aureus strains. The choice between these agents should consider local resistance patterns and patient allergies, with combination therapy reserved for severe cases or treatment failures.
Opioid management for severe acute exacerbations
Severe pilonidal cyst pain may require short-term opioid therapy, particularly during acute exacerbations or following surgical interventions. Codeine phosphate 30-60mg every 4-6 hours provides moderate pain relief with relatively low abuse potential, though genetic variations in metabolism can affect efficacy. For more severe pain, tramadol 50-100mg every 6 hours offers both opioid and non-opioid mechanisms of action, potentially reducing the risk of tolerance development. Opioid prescriptions should be limited to 3-7 days for acute episodes, with clear patient education regarding proper use and disposal of unused medications.
Surgical intervention pain expectations and recovery timelines
Surgical intervention becomes necessary when conservative management fails or when pilonidal disease becomes recurrent and significantly impacts quality of life. Understanding post-surgical pain patterns and recovery expectations helps patients prepare for the healing process and make informed treatment decisions. The type of surgical procedure performed significantly influences both immediate post-operative discomfort and long-term pain outcomes.
Incision and drainage procedures, typically performed for acute abscesses, involve minimal tissue removal and generally result in moderate post-operative pain lasting 3-5 days. Patients can expect pain scores of 4-6 on the visual analogue scale during the first 48 hours, with gradual improvement thereafter. The procedure itself provides immediate pressure relief, though the initial surgical trauma may temporarily increase discomfort before the benefits become apparent.
Wide excision procedures, involving complete removal of the pilonidal sinus and surrounding tissue, result in more significant post-operative pain but offer lower recurrence rates. Pain intensity typically peaks within the first 24-48 hours post-surgery, with scores often reaching 6-8 on standardised scales. Recovery timelines for wide excision vary considerably depending on whether the wound is left open for secondary healing or closed primarily. Open wounds require 4-8 weeks for complete healing but are associated with less severe acute pain, while closed wounds heal within 2-3 weeks but may experience higher pain scores initially.
Minimally invasive procedures, such as endoscopic pilonidal sinus treatment, offer the advantage of reduced post-operative pain and faster recovery times. These techniques typically result in pain scores of 2-4 during the first week post-procedure, with most patients returning to normal activities within 7-14 days. The reduced tissue trauma associated with these approaches translates to less inflammatory response and consequently lower pain levels throughout the recovery period.
Modern surgical techniques for pilonidal disease have significantly reduced post-operative pain levels, with minimally invasive approaches showing 40-60% lower pain scores compared to traditional excision methods.
Pain management protocols for post-surgical patients typically involve a multimodal approach combining scheduled NSAIDs with as-needed opioid medications for breakthrough pain. The transition from prescription pain medications to over-the-counter options usually occurs within the first week post-surgery, though individual variation is common. Patients undergoing more extensive procedures may require longer courses of prescription analgesics, particularly during the initial wound healing phase.
Post-treatment pain management and recurrence prevention
Effective post-treatment pain management extends beyond the immediate recovery period, encompassing long-term strategies to prevent recurrence and manage chronic discomfort that may persist following treatment. The transition from acute to chronic pain patterns requires careful monitoring and adjustment of management strategies to maintain optimal quality of life and functional status.
Long-term pain prevention strategies focus primarily on addressing the underlying factors that contribute to pilonidal disease development. Regular hair removal from the natal cleft area remains the most effective preventative measure, with laser hair removal showing superior outcomes compared to traditional methods. Studies indicate that patients who undergo professional laser hair removal experience recurrence rates of less than 10% compared to 25-30% in those using conventional hair removal methods.
Chronic pain following pilonidal treatment affects approximately 15-20% of patients and may result from nerve damage, scar tissue formation, or persistent low-grade inflammation. Neuropathic pain medications such as gabapentin or pregabalin may be beneficial for patients experiencing persistent burning or shooting sensations in the treated area. These medications typically require 2-4 weeks to achieve therapeutic levels and optimal pain relief, with dosing titrated based on individual response and tolerance.
Scar tissue management plays a crucial role in preventing long-term discomfort and functional limitations. Regular massage of healed incision sites with moisturising creams can help maintain tissue flexibility and reduce adhesion formation. Silicone gel sheets applied to mature scars may also help reduce pain and improve cosmetic outcomes, though evidence for their effectiveness in the pilonidal region specifically is limited.
Activity modification and ergonomic considerations become particularly important for patients whose occupations involve prolonged sitting or exposure to pilonidal disease risk factors. The use of specialised cushions, regular position changes, and appropriate clothing selection can significantly reduce the likelihood of disease recurrence and associated pain episodes. Patients in high-risk occupations may benefit from workplace accommodations to reduce prolonged pressure on the sacrococcygeal region.
Follow-up care protocols should include regular assessment of pain levels, functional status, and signs of recurrence at 6-week,
3-month, and 12-month intervals. These assessments should evaluate healing progress, pain levels, and any signs of recurrence that might indicate the need for additional interventions. Patients experiencing persistent pain beyond 6 months post-treatment may benefit from referral to pain management specialists for comprehensive evaluation and advanced treatment options.
Psychological support becomes increasingly important for patients dealing with chronic pilonidal disease, as the condition can significantly impact mental health and social functioning. Cognitive behavioural therapy has shown promise in helping patients develop coping strategies for chronic pain and reducing the psychological burden associated with recurrent disease episodes. Support groups, either in-person or online, can provide valuable peer support and practical advice for managing the long-term challenges of pilonidal disease.
The integration of lifestyle modifications with medical treatment creates a comprehensive approach to pain management and recurrence prevention. Regular exercise, particularly activities that strengthen the core and improve posture, can help reduce pressure on the sacrococcygeal region. Dietary modifications to promote regular bowel movements and reduce straining during defecation may also contribute to overall comfort and healing. Weight management, when appropriate, can significantly reduce mechanical stress on the affected area and improve treatment outcomes.
Emerging therapies for post-treatment pain management include platelet-rich plasma injections and stem cell therapy, though these approaches remain largely experimental. Early clinical trials suggest potential benefits for patients with persistent pain following traditional treatments, but more research is needed to establish their safety and efficacy profiles. Patients interested in these innovative approaches should discuss the risks and benefits with their healthcare providers and consider participation in clinical trials when available.
Long-term success in pilonidal disease management depends not only on appropriate initial treatment but also on comprehensive post-treatment care and patient education regarding prevention strategies.
Regular monitoring of the treated area for signs of recurrence allows for early intervention when problems arise. Patients should be educated to recognise early warning signs such as increased pain, swelling, or discharge, as prompt treatment of recurrent disease can prevent progression to more severe complications. The establishment of clear communication channels with healthcare providers ensures that patients can access appropriate care when needed without unnecessary delays.
Technology-assisted monitoring, including smartphone applications for symptom tracking and telemedicine consultations, represents an emerging trend in post-treatment care. These tools can help patients maintain detailed records of their symptoms and recovery progress while providing healthcare providers with valuable data for optimising treatment protocols. The integration of wearable devices that monitor activity levels and postural patterns may also contribute to personalised prevention strategies in the future.
