Persistent sinus infections affect millions of people worldwide, transforming what should be a temporary inconvenience into a debilitating chronic condition. When conventional treatments fail to provide lasting relief, patients often find themselves trapped in a cycle of recurring symptoms, multiple antibiotic courses, and mounting frustration. Understanding why some sinus infections resist standard therapeutic approaches requires examining the complex interplay of anatomical factors, microbial resistance patterns, and underlying systemic conditions that perpetuate chronic rhinosinusitis.
The transition from acute to chronic sinusitis represents more than simply an extended timeline of symptoms. Chronic rhinosinusitis involves fundamental changes in sinus physiology, immune response, and bacterial ecology that make resolution increasingly difficult. Modern diagnostic techniques and therapeutic interventions offer hope for those suffering from treatment-resistant cases, but success often requires a comprehensive understanding of the underlying pathophysiology driving persistent inflammation.
Chronic sinusitis pathophysiology and anatomical complications
The development of chronic sinusitis involves a complex cascade of inflammatory processes that fundamentally alter normal sinus function. Unlike acute infections that typically resolve within days to weeks, chronic cases persist due to sustained inflammation of the paranasal sinus mucosa, which becomes thickened and oedematous. This chronic inflammatory state creates an environment conducive to bacterial colonisation and biofilm formation, perpetuating the infection cycle.
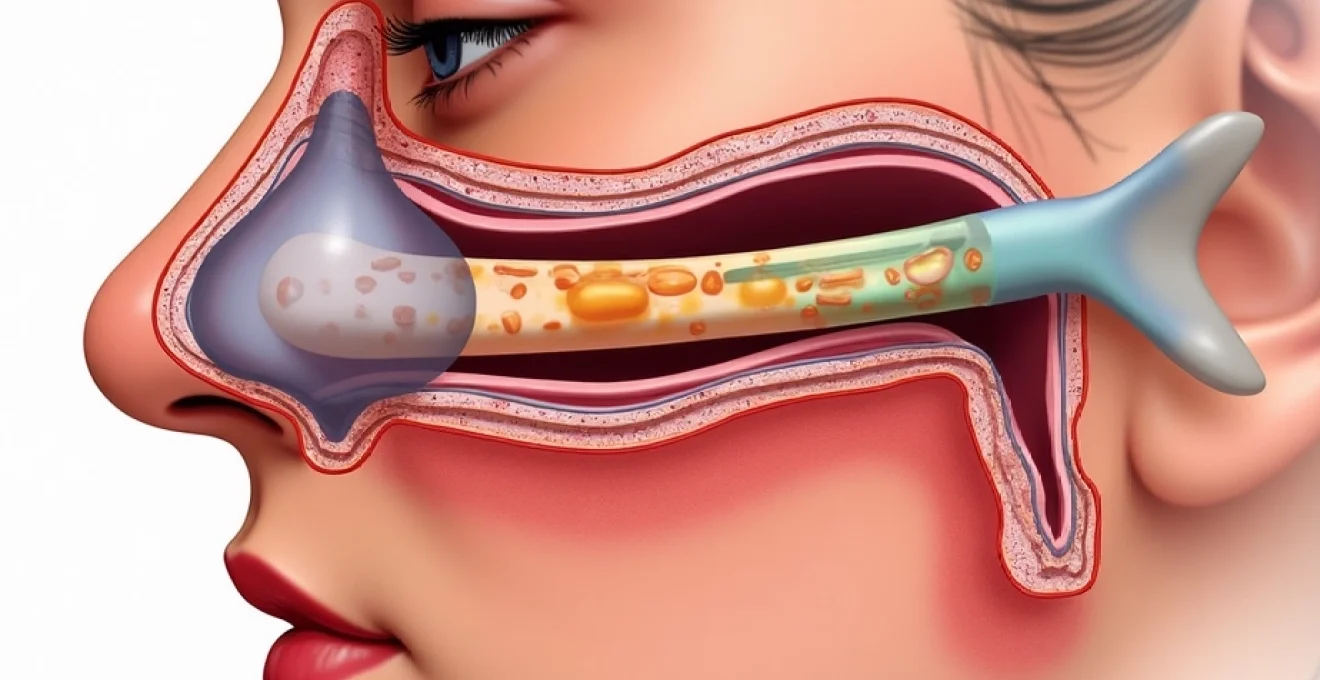
The normal sinuses function as air-filled cavities lined with ciliated respiratory epithelium that produces mucus to trap pathogens and debris. Coordinated ciliary action sweeps this mucus towards the natural ostia, maintaining sterile sinus cavities. However, in chronic sinusitis, this delicate balance becomes disrupted through multiple mechanisms, including ciliary dysfunction, mucus hypersecretion, and structural abnormalities that impede drainage.
Ostiomeatal complex obstruction and mucociliary dysfunction
The ostiomeatal complex represents the critical drainage pathway for the frontal, maxillary, and anterior ethmoid sinuses. This narrow anatomical region, measuring only 1-3 millimetres in width, becomes easily obstructed during inflammatory processes. When inflammation causes mucosal swelling within this confined space, it creates a cascade effect that impacts multiple sinus cavities simultaneously.
Mucociliary dysfunction plays a pivotal role in perpetuating chronic infections. The normal ciliary beat frequency of 1000-1500 beats per minute becomes significantly reduced in chronically inflamed tissue, dropping to as low as 200-400 beats per minute. This dramatic reduction in ciliary activity severely compromises the sinus’s ability to clear pathogens and inflammatory debris, creating stagnant pools of infected mucus that serve as reservoirs for persistent infection.
Biofilm formation in paranasal sinuses
Recent research has identified bacterial biofilms as a major factor in treatment-resistant chronic sinusitis. These complex microbial communities become embedded within a protective extracellular matrix that shields bacteria from both host immune responses and antimicrobial agents. Studies indicate that biofilms are present in 75-90% of chronic sinusitis cases, explaining why conventional antibiotic therapy often fails to achieve lasting cure.
The biofilm lifestyle provides bacteria with significant survival advantages, including increased resistance to antibiotics (up to 1000-fold higher than planktonic bacteria), protection from phagocytic cells, and enhanced ability to persist in hostile environments. Common biofilm-forming organisms in chronic sinusitis include Pseudomonas aeruginosa , Staphylococcus aureus , and Haemophilus influenzae , which often coexist in polymicrobial communities.
Deviated septum and concha bullosa impact on drainage
Structural abnormalities within the nasal cavity and paranasal sinuses significantly contribute to persistent infections by disrupting normal airflow patterns and mucus drainage. A deviated nasal septum, present in approximately 80% of the adult population to some degree, can create areas of stagnant air and impaired ventilation. When severe, septal deviation can completely obstruct sinus ostia, creating an anaerobic environment favourable to pathogenic bacterial growth.
Concha bullosa, or pneumatisation of the middle turbinate, occurs in 25-35% of individuals and can significantly impact ostiomeatal complex drainage. These air-filled turbinates can compress adjacent structures, narrowing drainage pathways and creating areas of recurrent obstruction. The combination of multiple structural abnormalities often requires surgical intervention to restore normal sinus physiology and achieve lasting symptom resolution.
Fungal rhinosinusitis and aspergillus fumigatus colonisation
Fungal involvement in chronic sinusitis represents a growing concern, particularly in immunocompromised patients or those with allergic predisposition. Aspergillus fumigatus and other saprophytic fungi can establish persistent colonisation within chronically inflamed sinuses, triggering intense eosinophilic inflammation and tissue remodelling. This fungal component often goes unrecognised in conventional bacterial culture-based diagnostics, leading to treatment failures when antifungal therapy is not incorporated.
Allergic fungal sinusitis (AFS) represents a distinct entity characterised by thick, eosinophilic mucin containing fungal elements and Charcot-Leyden crystals. Patients with AFS typically demonstrate elevated total IgE levels, positive fungal-specific IgE, and may have concurrent asthma or nasal polyposis. The inflammatory cascade triggered by fungal antigens creates a self-perpetuating cycle that requires both surgical debridement and long-term antifungal therapy for optimal management.
Resistant bacterial pathogens in refractory sinus infections
The emergence of antibiotic-resistant bacterial pathogens represents one of the most significant challenges in treating persistent sinus infections. Unlike acute sinusitis, which typically responds to standard antimicrobial therapy, chronic cases often harbour multidrug-resistant organisms that have developed sophisticated mechanisms to evade both immune responses and therapeutic interventions. Understanding the specific resistance patterns and virulence factors of these pathogens is crucial for developing effective treatment strategies.
The prolonged course of chronic sinusitis, combined with repeated antibiotic exposures, creates selective pressure that favours resistant bacterial strains. This microbial evolution occurs within the protected environment of infected sinuses, where suboptimal antibiotic penetration and biofilm formation provide additional survival advantages. The result is often a polymicrobial infection dominated by highly resistant organisms that require specialised diagnostic techniques and targeted therapeutic approaches.
Methicillin-resistant staphylococcus aureus (MRSA) sinusitis
MRSA has emerged as a significant pathogen in chronic sinusitis, particularly in patients with previous healthcare exposures or immunocompromising conditions. The prevalence of MRSA in chronic sinusitis ranges from 8-15% in community settings and can exceed 30% in nosocomial infections. These organisms demonstrate resistance not only to beta-lactam antibiotics but often exhibit multidrug resistance patterns that significantly limit therapeutic options.
The pathogenesis of MRSA sinusitis involves multiple virulence factors, including protein A, which interferes with opsonisation and phagocytosis, and various toxins that cause tissue damage and inflammation. MRSA strains often produce biofilms that are particularly robust and difficult to eradicate, requiring prolonged courses of biofilm-penetrating antibiotics such as linezolid, daptomycin, or tigecycline. The treatment duration typically extends 4-6 weeks, compared to 10-14 days for standard bacterial sinusitis.
Extended-spectrum Beta-Lactamase producing enterobacteriaceae
Extended-spectrum beta-lactamase (ESBL) producing organisms have become increasingly problematic in chronic sinusitis, particularly following multiple courses of broad-spectrum antibiotics. These enzymes confer resistance to most beta-lactam antibiotics, including third-generation cephalosporins and aztreonam. Common ESBL producers in sinus infections include Klebsiella pneumoniae , Escherichia coli , and Enterobacter species.
The detection of ESBL-producing organisms requires specialised laboratory techniques, as standard susceptibility testing may not accurately reflect clinical resistance. Treatment typically requires carbapenem antibiotics, although increasing rates of carbapenemase production among these organisms pose additional therapeutic challenges. The emergence of colistin resistance in some ESBL producers has created scenarios where few or no effective oral antibiotic options remain available.
Pseudomonas aeruginosa and anaerobic polymicrobial infections
Pseudomonas aeruginosa represents one of the most challenging pathogens in chronic sinusitis due to its intrinsic antibiotic resistance and exceptional biofilm-forming capacity. This organism produces multiple virulence factors, including elastase, phospholipase C, and pyocyanin, which contribute to tissue destruction and chronic inflammation. The ability of P. aeruginosa to rapidly develop resistance during treatment makes eradication particularly difficult.
Anaerobic bacteria often coexist with Pseudomonas in chronic infections, creating complex polymicrobial communities. Common anaerobes include Prevotella , Fusobacterium , and Bacteroides species, which thrive in the low-oxygen environment of obstructed sinuses. These organisms produce enzymes that inactivate beta-lactam antibiotics and create an inflammatory milieu that perpetuates tissue damage. Effective treatment requires antibiotics with both aerobic and anaerobic coverage, such as piperacillin-tazobactam or metronidazole combinations.
Antibiotic-resistant streptococcus pneumoniae strains
Penicillin-resistant Streptococcus pneumoniae (PRSP) has become increasingly prevalent in chronic sinusitis, with resistance rates exceeding 25% in many geographic regions. These organisms demonstrate varying levels of penicillin resistance, from intermediate (MIC 0.1-1.0 μg/ml) to high-level resistance (MIC ≥2.0 μg/ml). Cross-resistance to other antibiotics, including macrolides, tetracyclines, and fluoroquinolones, often complicates treatment selection.
The mechanism of pneumococcal resistance involves alterations in penicillin-binding proteins (PBPs), which reduce antibiotic affinity and effectiveness. High-dose amoxicillin remains effective against many PRSP strains due to the high concentrations achieved in sinus tissue, but resistant strains may require alternative agents such as respiratory fluoroquinolones or ceftriaxone. The emergence of fluoroquinolone-resistant pneumococci has further limited oral treatment options for these infections.
Underlying systemic conditions perpetuating chronic rhinosinusitis
Many cases of treatment-resistant chronic sinusitis stem from underlying systemic conditions that compromise normal sinus physiology or immune function. These conditions create an environment where standard therapeutic approaches fail to achieve lasting resolution, as the underlying pathophysiology remains unaddressed. Recognition and management of these systemic factors is often crucial for achieving successful long-term outcomes in challenging cases.
The relationship between systemic disease and chronic sinusitis is bidirectional, with sinus inflammation potentially exacerbating underlying conditions while systemic disease perpetuates sinus pathology. This complex interplay requires a comprehensive diagnostic approach that extends beyond local sinus pathology to evaluate potential systemic contributors. Early identification of these conditions can dramatically improve treatment outcomes and prevent unnecessary repeated interventions.
Primary ciliary dyskinesia and kartagener syndrome
Primary ciliary dyskinesia (PCD) represents a rare but important cause of chronic sinusitis, affecting approximately 1 in 16,000 individuals. This genetic disorder involves defects in ciliary ultrastructure or function, leading to impaired mucociliary clearance throughout the respiratory tract. Patients with PCD typically present with chronic sinusitis from early childhood, often accompanied by chronic productive cough, recurrent pneumonia, and bronchiectasis.
Kartagener syndrome, a subset of PCD affecting about 50% of patients, includes the classic triad of chronic sinusitis, bronchiectasis, and situs inversus. The diagnosis requires specialised testing, including nasal nitric oxide measurement, ciliary biopsy with electron microscopy, and genetic testing for known PCD mutations. Treatment focuses on enhancing mucociliary clearance through airway hygiene techniques, anti-inflammatory medications, and aggressive management of secondary infections.
Cystic Fibrosis-Associated sinusitis and CFTR mutations
Cystic fibrosis (CF) causes universal involvement of the paranasal sinuses, with 90-100% of patients developing chronic rhinosinusitis. The defective CFTR protein leads to abnormal chloride transport and subsequent mucus dehydration, creating thick, viscous secretions that are difficult to clear. This environment promotes bacterial colonisation, particularly with Pseudomonas aeruginosa and Staphylococcus aureus , often in biofilm configurations.
CF-associated sinusitis typically presents with nasal polyposis, anosmia, and chronic purulent discharge. The condition often requires aggressive medical management including mucolytics, hypertonic saline irrigation, and prolonged antibiotic courses. Surgical intervention may be necessary but requires careful consideration of the patient’s overall pulmonary status and life expectancy. CFTR modulators such as ivacaftor and lumacaftor have shown promise in improving sinus symptoms by addressing the underlying protein dysfunction.
Aspirin-exacerbated respiratory disease (samter’s triad)
Aspirin-exacerbated respiratory disease (AERD), previously known as Samter’s triad, affects 2-9% of adults with asthma and involves the classic combination of asthma, chronic rhinosinusitis with nasal polyposis, and reactions to aspirin and other NSAIDs. The condition results from dysregulated arachidonic acid metabolism, leading to overproduction of cysteinyl leukotrienes and underproduction of protective prostaglandins.
Patients with AERD typically experience severe, recalcitrant nasal polyposis that rapidly recurs following surgical removal. The chronic inflammation is characterised by intense eosinophilic infiltration and tissue remodelling that responds poorly to standard therapies. Management requires a comprehensive approach including leukotriene receptor antagonists, high-dose topical corticosteroids, and often aspirin desensitisation therapy. Biologic agents targeting the IL-5 pathway, such as mepolizumab and benralizumab, have shown significant efficacy in reducing polyp burden and improving quality of life.
Immunoglobulin deficiency syndromes and recurrent infections
Primary immunodeficiency disorders predispose patients to recurrent and chronic sinus infections that often resist standard treatment approaches. Common variable immunodeficiency (CVID) represents the most frequent clinically significant primary immunodeficiency, affecting 1 in 25,000-50,000 individuals. Patients typically present with recurrent bacterial infections of the respiratory tract, including chronic sinusitis, due to defective antibody production.
Selective IgA deficiency, affecting 1 in 500-700 individuals, may also contribute to chronic sinusitis, particularly when combined with IgG subclass deficiencies. These patients often experience recurrent infections with encapsulated bacteria such as Streptococcus pneumoniae and Haemophilus influenzae . Diagnosis requires comprehensive immunological evaluation including quantitative immunoglobulin levels, specific antibody responses to protein and polysaccharide antigens, and lymphocyte subset analysis. Treatment may require immunoglobulin replacement therapy and prophylactic antibiotics in addition to standard sinus management.
Advanced diagnostic imaging and laboratory assessment
Modern diagnostic approaches for treatment-resistant chronic sinusitis extend far beyond conventional radiographic imaging and culture-based microbiology. High-resolution computed tomography (HRCT) remains the gold standard for anatomical assessment, providing detailed visualisation of sinus anatomy, inflammatory changes, and potential surgical landmarks. However, magnetic resonance imaging (MRI) offers superior soft tissue characterisation and can differentiate between various types of inflammatory
secretions, fungal infections, and neoplastic processes that may mimic chronic inflammatory disease.Advanced laboratory assessment should include comprehensive microbiology with extended incubation periods to detect fastidious organisms, fungal cultures with speciation, and molecular diagnostic techniques such as 16S rRNA sequencing to identify unculturable bacteria. Histopathological examination of tissue specimens obtained during endoscopic procedures can reveal characteristic patterns associated with specific conditions, including allergic fungal sinusitis, granulomatous inflammation, or malignancy. Inflammatory biomarkers such as C-reactive protein, erythrocyte sedimentation rate, and specific cytokine profiles may provide insights into the underlying inflammatory mechanisms driving persistent disease.Flow cytometry analysis of sinonasal secretions can quantify various immune cell populations, including neutrophils, eosinophils, and T-cell subsets, helping to characterise the predominant inflammatory pathway. This information proves particularly valuable when selecting targeted biologic therapies for patients with eosinophilic or Th2-driven inflammatory patterns. Additionally, measurement of local IgE levels and specific allergen testing can identify environmental triggers that perpetuate chronic inflammation.
Therapeutic interventions for treatment-resistant cases
Management of treatment-resistant chronic sinusitis requires a multimodal approach that addresses the complex pathophysiology underlying persistent inflammation. Traditional antibiotic therapy often proves insufficient due to biofilm formation, resistant pathogens, and underlying structural or immunological abnormalities. Contemporary treatment strategies focus on combining targeted antimicrobial therapy with anti-inflammatory agents, mechanical disruption of biofilms, and correction of predisposing factors.
Topical therapy represents a cornerstone of modern chronic sinusitis management, as it delivers high concentrations of active medications directly to affected tissues while minimising systemic exposure. High-volume saline irrigation with hypertonic solutions (3-7% sodium chloride) provides mechanical debridement of inflammatory debris and biofilms while creating an osmotic environment unfavourable to bacterial growth. The addition of antimicrobial agents such as mupirocin, gentamicin, or amphotericin B to irrigation solutions can enhance efficacy against resistant pathogens and fungal elements.
Corticosteroid therapy remains fundamental in managing the inflammatory component of chronic sinusitis. Topical corticosteroids delivered via high-volume irrigation or nebulisation achieve superior tissue penetration compared to traditional nasal sprays. Budesonide respules mixed with saline irrigation have demonstrated significant efficacy in reducing inflammatory markers and improving symptom scores. For severe cases, systemic corticosteroid courses may be necessary to achieve initial inflammatory control, although long-term use should be avoided due to potential adverse effects.
Biologic therapies represent a revolutionary advancement for patients with eosinophilic chronic rhinosinusitis and nasal polyposis. Dupilumab, a monoclonal antibody targeting the IL-4 receptor α subunit, blocks both IL-4 and IL-13 signalling pathways central to Th2-mediated inflammation. Clinical trials have demonstrated dramatic reductions in polyp burden, improvement in olfactory function, and decreased need for systemic corticosteroids. Other biologics targeting the IL-5 pathway, including mepolizumab and benralizumab, show particular promise for patients with severe eosinophilic disease and comorbid asthma.
Antimicrobial selection for treatment-resistant cases requires consideration of local resistance patterns, biofilm penetration capabilities, and patient-specific factors. Macrolide antibiotics demonstrate anti-inflammatory properties beyond their antimicrobial effects, making them particularly valuable in chronic cases. Clarithromycin and azithromycin can reduce inflammatory cytokine production and improve mucociliary function even in the absence of susceptible pathogens. For biofilm-disrupting therapy, combinations of antibiotics with different mechanisms of action may prove more effective than single-agent therapy.
Adjunctive therapies play an increasingly important role in comprehensive management. Mucolytic agents such as N-acetylcysteine and dornase alfa can improve mucus rheology and facilitate drainage. Leukotriene receptor antagonists provide additional anti-inflammatory effects, particularly in patients with comorbid asthma or aspirin sensitivity. Probiotics may help restore normal microbiome balance following intensive antibiotic therapy, although research in this area remains preliminary.
Endoscopic sinus surgery techniques and post-operative management
When medical therapy fails to achieve adequate symptom control, endoscopic sinus surgery (ESS) offers the potential for anatomical correction and improved access for topical therapies. Modern surgical techniques focus on preserving normal anatomy while removing diseased tissue and addressing structural abnormalities that impede drainage. The extent of surgery should be tailored to disease severity and patient-specific factors, ranging from limited procedures targeting specific anatomical problems to comprehensive approaches addressing all affected sinus cavities.
Functional endoscopic sinus surgery techniques have evolved significantly with improved instrumentation and image guidance systems. Computer-assisted navigation allows for precise localisation of critical structures and enhances safety during complex procedures. Balloon catheter dilation represents a minimally invasive option for patients with isolated ostiomeatal complex obstruction, offering reduced morbidity compared to traditional tissue removal techniques. However, this approach may not be suitable for patients with extensive polyposis or fungal disease requiring comprehensive debridement.
The concept of “reboot surgery” has emerged for patients with severe chronic rhinosinusitis, involving complete removal of diseased mucosa followed by intensive topical therapy during the healing period. This approach aims to eliminate established biofilms and inflammatory tissue while creating a clean environment for mucosal regeneration. Post-operative management becomes crucial for success, requiring aggressive saline irrigation, topical corticosteroids, and often culture-directed antibiotic therapy based on intraoperative specimens.
Extended frontal sinus procedures may be necessary for patients with refractory frontal sinusitis, including frontal sinusotomy, Draf II procedures, or the modified endoscopic Lothrop procedure (Draf III). These techniques require significant expertise due to the proximity of critical structures including the anterior skull base and orbit. Long-term patency rates depend heavily on post-operative care and the underlying disease process driving inflammation.
Post-operative management represents a critical determinant of surgical success in chronic sinusitis patients. Early and aggressive saline irrigation helps prevent synechiae formation and promotes healing. The timing and intensity of irrigation protocols should be individualised based on the extent of surgery and patient tolerance. Topical corticosteroids should be initiated early in the post-operative period, with high-volume delivery systems preferred over traditional nasal sprays for enhanced tissue penetration.
Regular endoscopic follow-up allows for early identification of complications such as synechiae, retained secretions, or recurrent polyposis. Minor adhesions can often be addressed in the office setting using flexible endoscopy, avoiding the need for revision surgery. Culture-directed antibiotic therapy may be necessary if signs of bacterial infection develop during the healing period, with selection based on intraoperative culture results and local resistance patterns.
The success of endoscopic sinus surgery in chronic rhinosinusitis depends on careful patient selection, appropriate surgical technique, and comprehensive post-operative care. While surgery can provide significant symptom relief and improved quality of life, it should be viewed as one component of a comprehensive management strategy rather than a definitive cure. Long-term success often requires ongoing medical therapy to control the underlying inflammatory process and prevent disease recurrence.
