Jock itch, medically termed tinea cruris, represents one of the most prevalent superficial fungal infections affecting the inguinal region. This dermatophyte infection impacts millions of individuals annually, with particularly high incidence rates in tropical and humid climates where optimal fungal growth conditions persist. Understanding the visual progression of healing provides patients and healthcare providers with crucial insights into treatment efficacy and expected recovery timelines.
The healing process of jock itch follows a predictable pattern of inflammatory resolution, tissue repair, and barrier restoration. Visual documentation during recovery serves as an invaluable tool for monitoring therapeutic progress and identifying potential complications. Recognising the distinct stages of healing enables more precise treatment adjustments and improved patient outcomes. This comprehensive visual guide examines each phase of recovery, from initial inflammatory presentation through complete resolution and potential post-inflammatory changes.
Understanding tinea cruris: pathophysiology and clinical manifestations
Tinea cruris develops through dermatophyte invasion of the stratum corneum, the outermost layer of skin in the inguinal region. The pathophysiology involves enzymatic breakdown of keratin by fungal organisms, leading to characteristic inflammatory responses and tissue damage. Understanding this process proves essential for recognising healing patterns and predicting recovery outcomes.
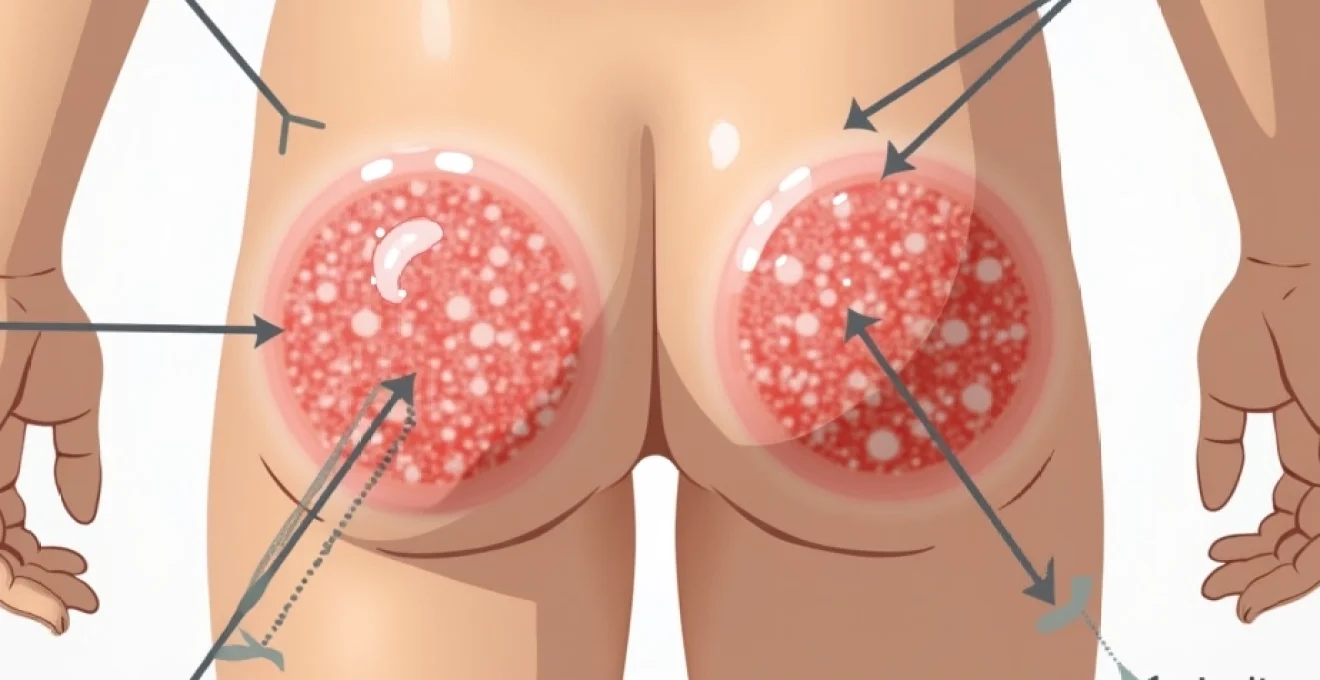
The clinical presentation typically manifests as erythematous, scaly patches with well-defined borders and central clearing. These lesions demonstrate a predilection for warm, moist areas including the groin creases, inner thighs, and occasionally extending to the buttocks and lower abdomen. The infection characteristically spares the scrotum and penile shaft, distinguishing it from candidal infections which commonly involve these areas.
Dermatophyte species identification: trichophyton rubrum vs epidermophyton floccosum
The two primary causative organisms demonstrate distinct clinical presentations and healing patterns. Trichophyton rubrum infections typically produce more inflammatory lesions with pronounced erythema and scaling, whilst Epidermophyton floccosum tends to create less inflammatory presentations with subtle border definition. Understanding these species-specific characteristics influences treatment selection and expected healing timelines.
Microscopic examination reveals septate hyphae and arthroconidia within infected tissue. The inflammatory response varies considerably between species, with T. rubrum generally producing more robust immune reactions and consequently more dramatic healing transformations. Visual documentation becomes particularly valuable in distinguishing between species-related healing patterns and potential treatment resistance.
Anatomical distribution patterns in the inguinal region
The anatomical distribution of tinea cruris follows predictable patterns based on moisture retention and friction exposure. Primary involvement typically begins in the inguinal creases, where occlusion and maceration create optimal fungal growth conditions. Secondary spread occurs along the medial thigh surfaces, following skin fold patterns and areas of clothing friction.
Understanding these distribution patterns proves crucial for visual healing assessment. Complete resolution requires clearance from all affected anatomical sites , not merely the most symptomatic areas. Sequential photographic documentation should encompass the entire distribution pattern to accurately monitor treatment progress and identify persistent infection foci.
Immunocompromised presentations and atypical morphology
Immunocompromised patients frequently demonstrate atypical presentations with extensive distribution, reduced inflammatory responses, or unusual morphological characteristics. These variations significantly impact healing patterns and visual documentation requirements. Diabetic patients, for instance, may exhibit delayed healing with prolonged inflammatory phases and increased risk of secondary bacterial infection.
Atypical presentations may lack the characteristic central clearing or demonstrate unusual pigmentation patterns during healing. Visual documentation in these cases requires extended monitoring periods and careful attention to subtle changes that might indicate treatment resistance or disease progression. The healing process often extends beyond standard treatment durations, necessitating prolonged visual monitoring.
Differential diagnosis: erythrasma and candidal intertrigo
Accurate visual assessment requires differentiation from similar conditions affecting the inguinal region. Erythrasma, caused by Corynebacterium minutissimum, produces well-demarcated, brown-red patches without the scaling typical of dermatophyte infections. Under Wood’s lamp examination, erythrasma demonstrates coral-red fluorescence, providing definitive diagnostic confirmation.
Candidal intertrigo typically presents with bright erythema, satellite pustules, and involvement of the scrotum and penile shaft. The healing patterns differ significantly, with candidal infections showing more rapid resolution of erythema but potential for recurring satellite lesions. Visual documentation helps distinguish these healing patterns and ensures appropriate treatment continuation or modification.
Visual documentation of healing stages: Day-by-Day progression analysis
The healing process of jock itch follows a predictable sequence of visual changes that can be systematically documented and analysed. Understanding these stages enables healthcare providers to assess treatment efficacy, predict recovery timelines, and identify potential complications or treatment resistance. Each stage demonstrates characteristic visual markers that serve as benchmarks for therapeutic progress.
Standardised photographic documentation requires consistent lighting conditions, standardised positioning, and appropriate magnification to capture relevant clinical details. The healing progression typically spans 2-4 weeks with topical antifungal therapy, though individual variation exists based on infection severity, immune status, and treatment compliance. Daily visual assessment during the first week provides the most valuable prognostic information for treatment success.
Initial inflammatory phase: erythematous border characteristics
The initial healing phase begins within 48-72 hours of commencing antifungal therapy, marked by subtle changes in border definition and erythema intensity. The characteristic advancing border begins to show reduced activity, with decreased scaling and less pronounced elevation compared to untreated lesions. This phase represents the earliest visual indicator of treatment response and fungal growth inhibition.
During this stage, the central clearing may become more pronounced as fungal burden decreases and inflammatory mediators begin to resolve. The erythema typically shifts from bright red to a duller, less inflammatory appearance. Careful documentation of border characteristics provides crucial prognostic information regarding treatment efficacy and expected recovery duration.
Desquamation period: scale reduction and edge clarity
The desquamation period, typically occurring during days 3-7 of treatment, demonstrates marked reduction in surface scaling and improved edge definition. The characteristic “ring-like” appearance becomes more subtle as the active inflammatory border resolves. This stage often represents the most dramatic visual improvement, providing significant encouragement for continued treatment compliance.
Scale reduction follows a centripetal pattern, beginning at the lesion periphery and progressing inward. The remaining scale becomes finer and less adherent, eventually resolving completely in successfully treated cases. Visual documentation during this period should focus on scale distribution patterns and border definition changes, as these provide the most reliable indicators of therapeutic progress.
Re-epithelialisation process: pigmentation changes
The re-epithelialisation process involves restoration of normal skin architecture and barrier function. This stage typically commences during the second week of treatment and may continue for several weeks beyond clinical cure. Visual changes include normalisation of skin texture, resolution of surface irregularities, and gradual restoration of normal pigmentation patterns.
Pigmentation changes represent a normal component of the healing process, with temporary hyperpigmentation or hypopigmentation commonly observed. These changes result from inflammatory damage to melanocytes and typically resolve spontaneously over 3-6 months. Documentation of pigmentation changes helps distinguish normal healing from post-inflammatory complications or treatment-related side effects.
Complete resolution markers: skin barrier restoration
Complete resolution encompasses restoration of normal skin appearance, texture, and barrier function. Visual markers include uniform pigmentation, normal skin surface texture, and absence of scaling or inflammatory changes. This stage typically occurs 2-4 weeks after treatment initiation, though individual variation exists based on infection severity and host factors.
Barrier restoration involves normalisation of transepidermal water loss, pH levels, and antimicrobial peptide production. While these changes may not be visually apparent, they represent crucial functional recovery markers. Clinical examination should confirm absence of residual scaling, particularly at previously affected border areas where treatment resistance commonly occurs.
Post-inflammatory hyperpigmentation development
Post-inflammatory hyperpigmentation represents a common sequela of tinea cruris, particularly in individuals with darker skin types. This condition typically develops 2-4 weeks after active infection resolution and may persist for several months. The hyperpigmentation follows the original infection distribution pattern, providing a visual “map” of the previous fungal involvement.
The degree of hyperpigmentation correlates with initial infection severity and inflammatory response intensity. Visual documentation of pigmentation changes helps differentiate normal post-inflammatory sequelae from active infection recurrence or treatment failure. Patient education regarding expected pigmentation changes prevents unnecessary anxiety and promotes treatment compliance during the recovery period.
Antifungal treatment protocols and response monitoring
Effective treatment of jock itch requires appropriate antifungal selection, optimal dosing regimens, and systematic response monitoring. Visual documentation plays a crucial role in assessing treatment efficacy and identifying the need for therapeutic modifications. Understanding the mechanisms of action and expected response patterns for different antifungal agents enables more precise treatment planning and improved patient outcomes.
Treatment response monitoring should incorporate both subjective symptom assessment and objective visual documentation. The correlation between visual improvement and mycological cure varies considerably between different antifungal agents and individual patient factors. Systematic visual assessment protocols provide standardised benchmarks for treatment evaluation and comparison between different therapeutic approaches.
Topical azoles: clotrimazole and miconazole efficacy rates
Azole antifungals represent first-line therapy for uncomplicated jock itch, with clotrimazole and miconazole demonstrating cure rates of 80-90% in clinical trials. These agents work through inhibition of ergosterol synthesis, leading to fungal cell membrane disruption and organism death. Visual response typically begins within 3-5 days of treatment initiation, with progressive improvement over subsequent weeks.
Clotrimazole demonstrates superior penetration in keratinised tissues, while miconazole provides enhanced activity against certain dermatophyte species. Visual monitoring should focus on border definition changes and scale reduction as primary efficacy indicators. Failure to show visual improvement within 7-10 days may indicate treatment resistance or incorrect diagnosis, warranting therapeutic reassessment.
Allylamine preparations: terbinafine hydrochloride applications
Terbinafine hydrochloride demonstrates fungicidal activity through squalene epoxidase inhibition, resulting in more rapid clinical improvement compared to azole preparations. Visual response typically occurs within 2-3 days, with dramatic reduction in inflammatory changes and scaling. The superior efficacy profile makes terbinafine particularly valuable for extensive or resistant infections.
The rapid visual response to terbinafine provides early prognostic information regarding treatment success. Patients typically experience significant symptom relief within 48 hours, accompanied by visible reduction in erythema and scaling. Visual documentation during terbinafine therapy should focus on the speed of improvement rather than gradual progression, as the response pattern differs markedly from azole agents.
Systemic therapy indications: itraconazole and fluconazole
Systemic antifungal therapy becomes necessary in cases of extensive disease, treatment resistance, or immunocompromised states. Itraconazole and fluconazole demonstrate excellent efficacy for refractory jock itch, with cure rates exceeding 95% in clinical studies. Visual response to systemic therapy typically shows delayed onset but more comprehensive resolution compared to topical agents.
The visual response pattern to systemic therapy differs from topical treatment, often showing initial stabilisation followed by gradual improvement over several weeks. Documentation should focus on overall disease extent reduction rather than localised changes, as systemic therapy addresses the entire fungal burden simultaneously. Patient monitoring requires attention to potential systemic side effects alongside visual improvement assessment.
Combination therapy: Antifungal-Corticosteroid formulations
Combination formulations containing antifungal agents and mild corticosteroids provide rapid symptomatic relief whilst maintaining antifungal efficacy. These preparations demonstrate particular value in highly inflammatory presentations where patient comfort becomes a primary concern. Visual response typically shows rapid erythema reduction within 24-48 hours, followed by gradual antifungal effect over subsequent weeks.
The use of combination therapy requires careful visual monitoring to ensure fungal clearance alongside symptomatic improvement. Corticosteroids may mask ongoing infection, creating false impressions of treatment success. Visual documentation should focus on complete resolution of all inflammatory and infectious markers, not merely symptomatic improvement.
Recovery timeline expectations and prognostic indicators
Understanding expected recovery timelines provides crucial context for patient counselling and treatment planning. The healing process typically follows predictable patterns, though individual variation exists based on infection severity, host immune status, and treatment compliance. Visual documentation serves as an objective measure of recovery progress, supplementing subjective symptom assessment and providing prognostic indicators for treatment success.
The complete recovery timeline spans 2-6 weeks for most patients, with initial improvement visible within 3-5 days of appropriate treatment. Early visual response strongly predicts ultimate treatment success , whilst delayed improvement may indicate treatment resistance, incorrect diagnosis, or underlying host factors affecting recovery. Systematic visual assessment enables early identification of treatment failure and timely therapeutic modifications.
Clinical studies demonstrate that patients showing significant visual improvement within the first week of treatment have a 95% probability of complete cure within 4 weeks, whilst those showing minimal early response have success rates below 60%.
Prognostic indicators derived from visual assessment include border definition changes, scale reduction patterns, central clearing progression, and overall lesion size reduction. These objective measures provide more reliable treatment monitoring compared to subjective symptom assessment alone. The correlation between visual improvement and mycological cure approaches 90% for most antifungal agents, making visual documentation a valuable surrogate marker for treatment efficacy.
Individual factors significantly influence recovery timelines, including patient age, immune status, diabetes presence, obesity, and concurrent medications. Elderly patients and those with diabetes typically demonstrate prolonged healing phases with extended inflammatory periods. Visual documentation in these populations requires modified expectations and extended monitoring periods to accurately assess treatment response.
Recurrence prevention strategies and Long-Term management
Preventing jock itch recurrence requires comprehensive understanding of predisposing factors and implementation of targeted preventive strategies. Visual documentation during the recovery period provides insights into individual risk factors and susceptibility patterns that influence recurrence likelihood. Long-term management approaches must address both immediate cure and sustained prevention to optimise patient outcomes.
Recurrence rates for successfully treated jock itch range from 15-25% within the first year, with higher rates observed in patients with predisposing conditions such as diabetes, obesity, or hyperhidrosis. Visual patterns during initial healing often predict recurrence risk, with patients showing delayed resolution or atypical healing patterns demonstrating increased susceptibility to reinfection.
Environmental modification represents the most effective strategy for preventing jock itch recurrence, with proper hygiene practices reducing reinfection rates by up to 70% in high-risk populations.
Long-term visual monitoring protocols should include periodic assessment of previously affected areas, particularly during high-risk periods such as summer months or increased physical activity. Early detection of recurrent lesions enables prompt treatment initiation and prevents progression to extensive disease. Patient education regarding visual signs of early recurrence empowers self-monitoring and promotes timely intervention.
- Maintenance of optimal skin dryness through proper hygiene and moisture-wicking clothing
- Regular antifungal powder application in high-risk individuals during susceptible periods
- Prompt treatment of concurrent fungal infections such as athlete’s foot to prevent cross-contamination
- Weight management and diabetes control to reduce predisposing factor influence
Prophylactic antifungal therapy may benefit high-risk patients with frequent recurrences, though this approach requires careful consideration of resistance development and side effect profiles. Visual monitoring during prophylactic therapy focuses on early detection of breakthrough infections and assessment of preventive efficacy. The optimal duration of prophylactic therapy varies based on individual risk factors and seasonal variation patterns.
Photographic documentation standards for medical assessment
Standardised photographic documentation requires adherence to established protocols ensuring consistency, reproducibility, and clinical utility. Proper documentation techniques enable accurate treatment monitoring, facilitate consultation processes, and provide valuable medico-legal documentation. Understanding technical requirements and clinical standards
encompasses proper equipment selection, technical settings, and clinical positioning standards.
High-quality digital photography requires consistent lighting conditions, preferably using standardised medical photography equipment with controlled illumination. The camera should be positioned at a consistent distance from the lesion, typically 15-20 centimeters, with the affected area occupying approximately 60-70% of the frame. Consistent photographic parameters ensure accurate comparison between sequential images and enable reliable assessment of treatment progress.
Technical settings should include standardised white balance, appropriate depth of field to ensure complete lesion focus, and sufficient resolution for detailed analysis. ISO settings should remain below 400 to minimise noise, whilst aperture settings between f/8-f/11 provide optimal depth of field for dermatological documentation. The use of standardised colour references within each photograph enables accurate colour assessment across different viewing devices and printing systems.
Patient positioning requires standardisation to ensure consistent anatomical landmarks and lesion orientation between sequential photographs. The inguinal region should be exposed sufficiently to document the complete lesion extent, including border areas and surrounding normal skin. Privacy considerations necessitate careful positioning and draping techniques that maintain patient dignity whilst ensuring comprehensive clinical documentation.
Documentation frequency varies based on infection severity and treatment response patterns. Daily photography during the first week provides optimal monitoring for treatment response assessment, whilst weekly documentation suffices for stable, improving lesions. High-risk patients or those with atypical presentations may require more frequent documentation to identify early signs of treatment failure or complication development.
Image storage and management systems must comply with medical record standards, ensuring secure storage, appropriate access controls, and integration with electronic health records. Standardised naming conventions should incorporate patient identifiers, anatomical location, and chronological sequence information. The documentation system should enable easy retrieval and comparison of sequential images for treatment monitoring and consultation purposes.
Quality assurance protocols should include regular equipment calibration, standardised lighting verification, and periodic review of documentation standards compliance. Training programs for healthcare personnel ensure consistent documentation techniques and appropriate patient interaction during the photography process. Regular audit of photographic documentation quality maintains clinical utility and enables continuous improvement of documentation protocols.
